fetal Engineered biologic matrix
TWENTY YEARS OF PROVEN clinical SAFETY AND PERFORMANCE
Fetal Engineered Biologic Matrix (f-EBM) was originally developed by Tissue Engineering Inc. (TEI), now Integra Lifesciences, and has been employed in many surgical indications since 2003. As an implantable medical device in critical applications such as dura mater repair, hernia repair, and plastic and reconstructive surgery, f-EBM has a rich heritage of exceptional clinical safety and performance.

Leveraging the unique properties of fetal and neonatal bovine dermis for cardiovascular indications
Harnessing the power of collagen type III
f-EBM is the only biologic matrix containing abundant levels of collagen Type III. Collagen Type III is involved in “scarless healing” observed in fetal and neonatal mammals. Implanted fetal collagen matrix, provides signals to a variety of cell surface receptors stimulating tissue regeneration and attenuating fibrosis.
Strength without crosslinking
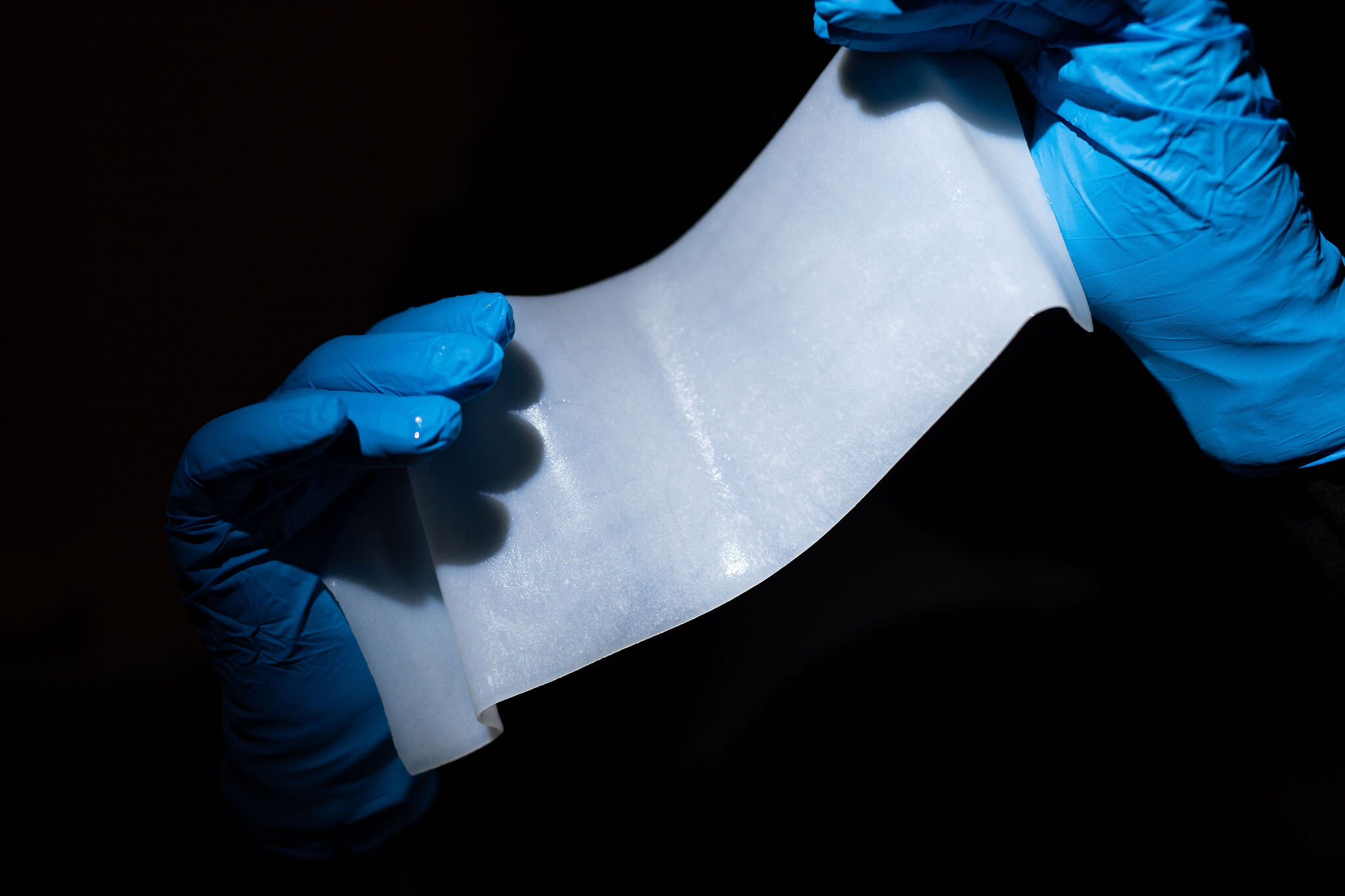
With a 3-dimensional network of collagen fibers, dermis is extremely strong, capable of withstanding both elevated tearing and suture stresses. In fact, bovine dermis is one of the strongest (refs. 1, 2, 3), soft biomaterials known, providing mechanical strength without employing crosslinking technologies. Although strong, f-EBM is highly conformable and has excellent surgical handling characteristics.
exceptional Purity
Our patented tissue engineering processes produce an exceptionally pure collagen scaffold, free of non collagen proteins, lipids, growth factors, or other inflammatory cellular remnants.
Angiogenesis and tissue regeneration
As a natural acellular scaffold with Type III collagen regenerative signalling, f-EBM displays both the ability to become repopulated with host cells, and to stimulate angiogenesis, a prerequisite for maturation of the matrix into functional host tissue (refs. 4, 5).
unmatched range of thicknesses
Different surgical situations can require different material thicknesses depending the requirements for ultimate tensile strength, anatomical location, and conformability. f-EBM provides surgeons with a market leading choice of formats ranging from less than 0.5 mm to more than 4 mm in thickness.
exceptional Surgical Usability
f-EBM is supplied dry but hydrates in room temperature saline in only 1-2 minutes with no disruption to standard surgical protocols. Once hydrated, f-EBM exhibits excellent handling characteristics, exhibiting flexibility and conformability without risking rippling during suturing. f-EBM’s class-leading suture retention strength provides surgeons a matrix they love to work with.
An ideal matrix for stem cell research
The cell-friendly environment of a non-crosslinked, 3-dimensional scaffold, combined with the regenerative signalling of collagen Type III, provides an ideal matrix for stem cell research. Furthermore, the natural porosity and thicknesses of fetal bovine dermis provides a large cell loading capacity.
Previous work (refs. 6, 7) has shown that human mesenchymal cells can proliferate within the f-EBM matrix and migrate to surrounding myocardial tissue. This opens up many possibilities for treating intractable diseases such as heart failure.
high absorbance capacity for pharmacotherapies
Due to the sponge-like nature of f-EBM, large quantities of drugs can be formulated within the 3-dimensional structure of the scaffold. Combining the natural strength and tissue friendliness of -fEBM together with the high loading capacity for a variety of active pharmaceutical ingredients, f-EBM serves as an ideal matrix for research-based local delivery of drugs to tissues.
References
1 Deeken CR, et al. “Differentiation of Biologic Scaffold Materials Through Physicomechanical, Thermal, and Enzymatic Degradation Techniques:” Annals of Surgery 255, 3: 595–604.
2 Neethling WML, Puls K, Rea A. Comparison of physical and biological properties of CardioCel with commonly used bioscaffolds. Interact Cardiovasc Thorac Surg. 2018;26:985-992.
3 Gallon A, Ph D, Goodchild T, Ph D, Wang R, Matheny RG. Remodeling of Extracellular Matrix Patch used for Carotid Artery Repair. J Surg Res. 2012;175(1):e25-e34.
4 Adelman, David M., and Kevin G. Cornwell. “Bioprosthetic Versus Synthetic Mesh: Analysis of Tissue Adherence and Revascularization in an Experimental Animal Model.” Plastic and Reconstructive Surgery - Global Open 6, no. 5 (May 2018): e1713.
5 Adelman, David M., and Kevin G. Cornwell. “Fundamentals of Extracellular Matrix Biomaterial Assimilation: Effect of Suture Type on Attachment Strength and Cell Repopulation.” Plastic and Reconstructive Surgery – Global Open 8, no. 3 (March 2020): e26354
6 Kouris NA, Squirrell JM, Jung JP, Pehlke CA, Hacker T, Eliceiri KW, Ogle BM. A nondenatured, noncrosslinked collagen matrix to deliver stem cells to the heart. Regenerative medicine. 2011 Sep;6(5):569-82.
7 Freeman BT, Kouris NA, Ogle BM. Tracking fusion of human mesenchymal stem cells after transplantation to the heart. Stem cells translational medicine. 2015 Jun;4(6):685-94.








